Few initiatives test a health plan's operational resilience like a core claims system implementation. According to research from McKinsey and the University of Oxford, 66% of enterprise software projects experience cost overruns, and 17% go so badly they threaten the organization's existence.¹ For health plans implementing QNXT, the stakes include regulatory compliance, provider relationships, and member satisfaction—all at risk if the project goes sideways.
The good news: most implementation failures are preventable. Understanding where projects typically break down allows health plans to plan proactively and avoid the most common pitfalls.
Data Migration and Conversion Complexity
Every QNXT implementation begins with a deceptively simple question: how do we move our data? The answer is never straightforward. Legacy claims systems store member information, provider records, and historical claims in formats that rarely align with QNXT's data model. Mapping decades of accumulated data—complete with inconsistencies, duplicates, and outdated codes—requires meticulous planning.
The risks are significant. Incomplete member histories create gaps in care coordination. Misaligned provider data leads to incorrect reimbursements. Claims history errors trigger audit findings and compliance exposure.
What works: Successful migrations follow a phased approach. Extract and profile legacy data early to understand its quality and structure. Build robust mapping rules with input from both technical staff and business users who understand the data's context. Validate extensively in parallel testing environments before cutover—identifying discrepancies in a test environment costs far less than fixing them in production. Budget adequate time for data cleansing; it almost always takes longer than planned.
Benefit Configuration Complexity
QNXT's flexibility is both its greatest strength and its most significant implementation hurdle. Configuring benefits correctly requires understanding the interplay between plan-level and product-level settings, accumulator logic, coordination of benefits rules, and state-specific requirements for Medicaid and Medicare Advantage populations.
Configuration errors rarely surface immediately. They emerge weeks or months later as claims adjudicate incorrectly, members receive wrong explanations of benefits, or accumulators fail to track properly toward deductibles and out-of-pocket maximums. By then, the remediation effort compounds exponentially.
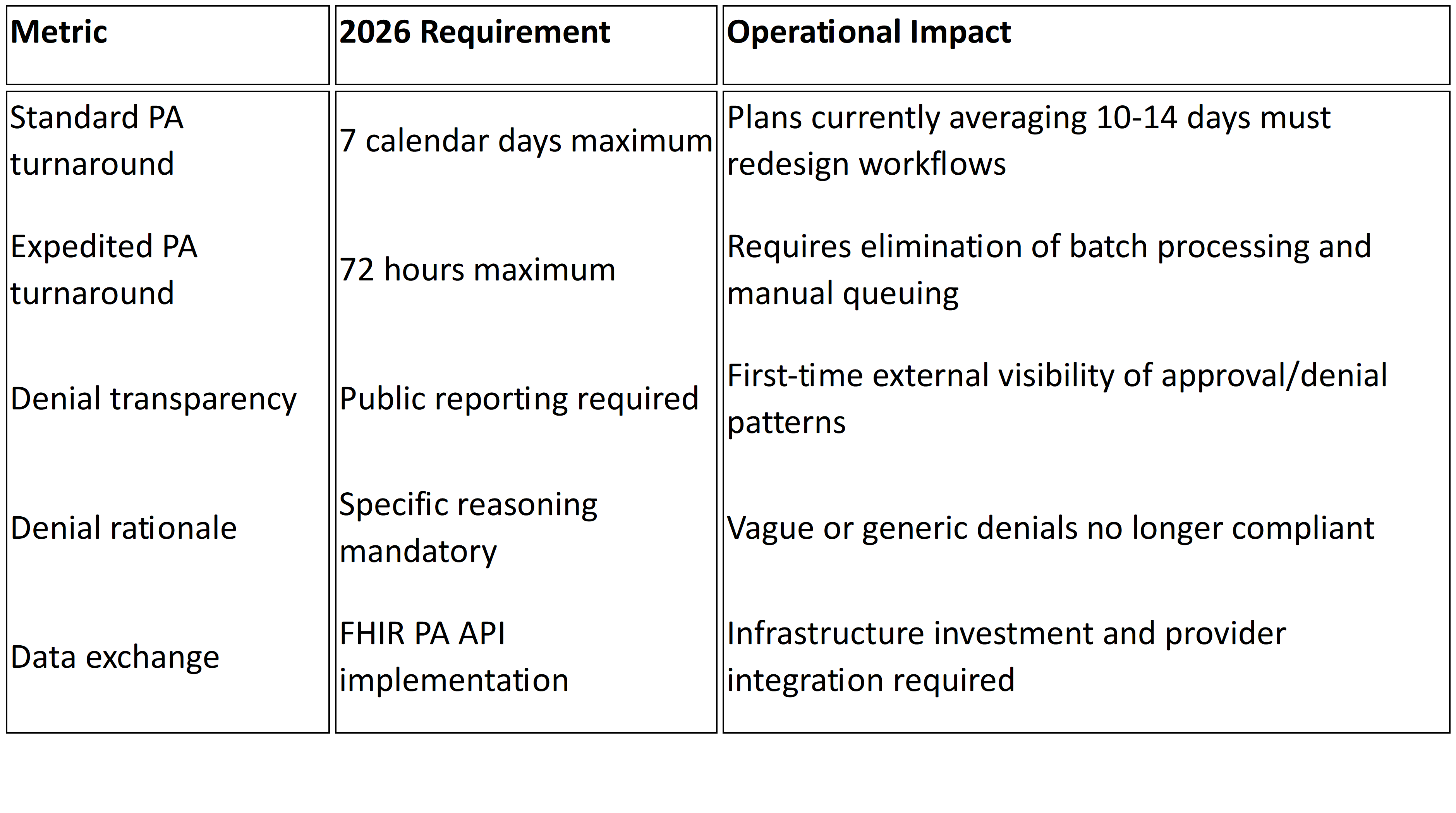
What works: Prioritize your highest-volume, highest-risk benefit configurations for early testing. Build comprehensive test case libraries that cover edge cases—not just the happy path. Document configuration decisions as you make them; institutional knowledge disappears quickly when team members move on. Engage business analysts who understand both the regulatory requirements and QNXT's configuration nuances. For Medicaid and Medicare Advantage plans, involve compliance staff early to ensure configurations align with CMS requirements.
Auto-Adjudication Rate Optimization
Go-live is just the beginning. Many health plans discover that their auto-adjudication rates plummet after implementing QNXT. The industry standard benchmark for auto-adjudication hovers around 80%, with best practice targets above 85%.² Yet many organizations fall short, with first-pass rates ranging from 10% to 70%.³
The financial impact is substantial. An auto-adjudicated claim costs health insurers cents on the dollar, while one requiring human intervention costs approximately $20.⁴ Every claim that falls out of auto-adjudication strains examiner capacity and extends turnaround times.
Low auto-adjudication rates typically stem from a few root causes: overly conservative editing rules, incomplete provider data, poorly configured fee schedules, or business rules that don't account for real-world claim variations. The system works as configured—the configuration simply doesn't reflect operational reality.
What works: Analyze pend patterns weekly in the months following go-live. Identify which edits generate the most fallout and assess whether they're truly necessary or just overly cautious defaults. Tune provider matching logic to reduce false pends from minor data discrepancies. Refine authorization integration so valid authorizations are properly recognized. Establish a continuous improvement cycle rather than treating go-live as the finish line.
Integration with Your Existing Ecosystem
QNXT doesn't operate in isolation. It must connect with EDI gateways for 837, 835, 834, and 270/271 transactions. It needs interfaces to provider portals, member platforms, care management systems, and payment integrity vendors. Each integration point introduces complexity—and potential failure modes.
The challenge intensifies when health plans operate hybrid environments during transition periods. Data must flow correctly between legacy and new systems without duplication, loss, or timing mismatches. Real-time authorization lookups must perform at production scale. Provider directories must stay synchronized across platforms.
Research shows that 51% of companies experience operational disruptions when going live with new enterprise systems, often due to integration failures.⁵
What works: Start integration testing earlier than you think necessary. Build end-to-end test scenarios that simulate production volumes and edge cases. Document every interface specification and establish clear ownership for each connection. Consider middleware layers to buffer complexity, but account for the latency and additional failure points they introduce. Plan for a parallel processing period where both old and new systems run simultaneously, allowing you to validate results before fully cutting over.
Training, Change Management, and Staffing Gaps
Even a perfectly configured QNXT instance fails if your people can't use it effectively. Research indicates that up to 75% of the financial benefits from new enterprise systems are directly linked to effective organizational change management—yet many organizations allocate less than 10% of their total project budget to this critical area.⁶
Implementation partners eventually leave. Institutional knowledge walks out the door. Claims examiners, configuration analysts, and IT staff must internalize new workflows, screens, and processes—often while maintaining production on legacy systems.
The training gap is particularly acute for configuration roles. QNXT benefit configuration requires specialized expertise that takes months to develop. Many health plans underestimate this learning curve and find themselves dependent on external consultants long after go-live.
What works: Build knowledge transfer into implementation contracts from day one. Document configuration decisions and create runbooks for common scenarios. Identify internal staff for intensive mentorship during the project—not just attendance at training sessions, but hands-on involvement in configuration work. Plan for productivity dips in the months following go-live and staff accordingly. Consider whether supplemental staffing can bridge capability gaps during the transition period rather than burning out your core team.
The Five Core QNXT Implementation Challenges
For quick reference, successful QNXT implementations address these critical areas:
- Data migration and validation — ensuring complete, accurate conversion from legacy systems through phased extraction, robust mapping, and extensive parallel testing
- Benefit configuration — methodical setup with comprehensive testing across all lines of business, with early compliance involvement for government programs
- Auto-adjudication optimization — continuous tuning post-go-live to maximize straight-through processing and reduce costly manual intervention
- System integration — reliable connections to EDI, portals, and downstream vendors, tested at production scale before cutover
- Training and change management — building internal expertise through hands-on involvement, not just classroom training, with realistic productivity expectations
Moving Forward
QNXT implementations are complex, but complexity doesn't have to mean chaos. Health plans that approach these projects with realistic timelines, thorough testing protocols, and genuine investment in their people consistently outperform those who underestimate the effort involved.
The patterns of failure are well-documented. So are the patterns of success. The difference usually comes down to preparation, honest assessment of internal capabilities, and willingness to invest in the areas—like change management and post-go-live optimization—that don't appear on the software license invoice but determine whether the project delivers value.
About Mizzeto
At Mizzeto, we help health plans navigate high-stakes platform transitions with the same rigor they apply to clinical and regulatory decisions. Our teams support QNXT implementations and optimization across Medicare, Medicaid, Exchange, and specialty lines of business—bridging strategy, configuration, and operational execution. The goal isn’t just a successful go-live, but durable performance: higher auto-adjudication, cleaner integrations, and internal teams equipped to govern the system long after consultants exit.
If your organization is preparing for a QNXT implementation—or working to stabilize and optimize one already in production—we’re always open to a thoughtful conversation.
Sources
- McKinsey & Company and BT Centre for Major Program Management at the University of Oxford. "Delivering Large-Scale IT Projects On Time, On Budget, and On Value." https://www.forecast.app/blog/66-of-enterprise-software-projects-have-cost-overruns
- Healthcare Finance News. "Claims processing is in dire need of improvement, but new approaches are helping." https://www.healthcarefinancenews.com/news/claims-processing-dire-need-improvement-new-approaches-are-helping
- HealthCare Information Management. "Understanding Auto Adjudication." https://hcim.com/understanding-auto-adjudication/
- Healthcare Finance News. "Claims processing is in dire need of improvement, but new approaches are helping." https://www.healthcarefinancenews.com/news/claims-processing-dire-need-improvement-new-approaches-are-helping
- RubinBrown ERP Advisory Services. "Top ERP Insights & Statistics." https://kpcteam.com/kpposts/top-erp-statistics-trends
- Sci-Tech-Today. "Enterprise Resource Planning (ERP) Software Statistics." https://www.sci-tech-today.com/stats/enterprise-resource-planning-erp-software-statistics/