Poor Data Integration in Utilization Management
In an industry increasingly defined by transformation, few areas of healthcare remain as inefficient and opaque as utilization management (UM). Originally designed as a gatekeeping function to ensure medical necessity and cost control, UM today often functions as a fragmented, manual process that creates more friction than value. Behind this dysfunction lies a core issue: poor data integration.
For payers, the result isn’t just operational waste. Fragmented UM workflows drive downstream denials, inflate appeals volume, and delay care decisions—hurting both the bottom line and member experience.
But it doesn't have to be this way. By reengineering how data flows through the UM process—particularly clinical, eligibility, and prior authorization data—health plans can unlock measurable gains in turnaround times, medical loss ratios, and member satisfaction.
The Current State: Friction at Every Turn
To understand the magnitude of the problem, consider a typical UM request. A provider faxes or uploads a prior authorization form to the payer. The clinical review team must manually check for eligibility, hunt down documentation in external systems, and review notes that often arrive in image or PDF format. Many plans lack direct access to relevant clinical history unless integrated with the provider’s EHR or a health information exchange. Even when data is available, systems often don’t talk to each other, requiring copy-paste workarounds and swivel-chair decision-making.
This isn't just inefficient—it’s dangerous. 78% of physicians reported that prior authorization often or sometimes results in their patients abandoning a recommended course of treatment, according to the American Medical Association (AMA)1. Behind many of these delays is the simple fact that UM reviewers don’t have the right data at the right time.
The Ripple Effect: Denials, Appeals, and Member Disruption
When data isn’t integrated, authorization requests are often incomplete. This leads to higher initial denial rates, often due to missing information, mismatched eligibility status, or failure to match clinical criteria—despite the service being medically necessary.
These denials create downstream work. Members are notified late. Providers resubmit documentation. Operations teams scramble to re-review the same cases. In some cases, services are delayed or denied altogether, forcing members into out-of-network options or emergency care.
The volume adds up. For a mid-size regional health plan processing over 500,000 UM requests annually, even a 5% increase in avoidable denials can translate to tens of thousands of rework cases—each one a cost center and a complaint waiting to happen.
What’s Missing: A Data Backbone for UM
UM doesn’t exist in isolation—it intersects with claims, member eligibility, provider networks, and clinical data. But most payer systems treat these as silos, not a unified operating model.
Three key gaps stand out:
- Eligibility and Benefits Data Not Embedded in UM Systems
UM reviewers often lack real-time visibility into a member’s active eligibility, benefits coverage, and network status—forcing them to toggle between systems or wait on back-office verification. - Clinical Data Unstructured or Inaccessible
Even when plans request clinical documentation, it often arrives as scanned images or PDF attachments that require manual review. Without structured clinical data—diagnoses, labs, medication history—automated triage and approval are nearly impossible. - Lack of Integration with Prior Auth Systems
Many plans rely on legacy prior auth platforms that don’t integrate with their case management, provider portals, or claims adjudication systems. This disconnect leads to mismatches in decisions versus payments.
Fixing the Flow: What Integrated UM Should Look Like
The fix is not about layering another portal on top. It’s about re-architecting the UM workflow around data integration, with a focus on real-time, bidirectional information exchange. Here’s what that looks like:
- Real-Time Eligibility Integration: UM platforms must have API-based access to core member data, pulling real-time eligibility, coverage, and benefit details directly into the authorization review workflow. This eliminates errors from outdated eligibility files and speeds up determinations.
- Structured Clinical Data Access: Rather than waiting for static faxes, plans should integrate with HIEs, EHRs, and data aggregators to receive structured clinical summaries. With proper NLP tools and smart forms, this data can be mapped into decision support tools that flag approvals or route complex cases to clinicians.
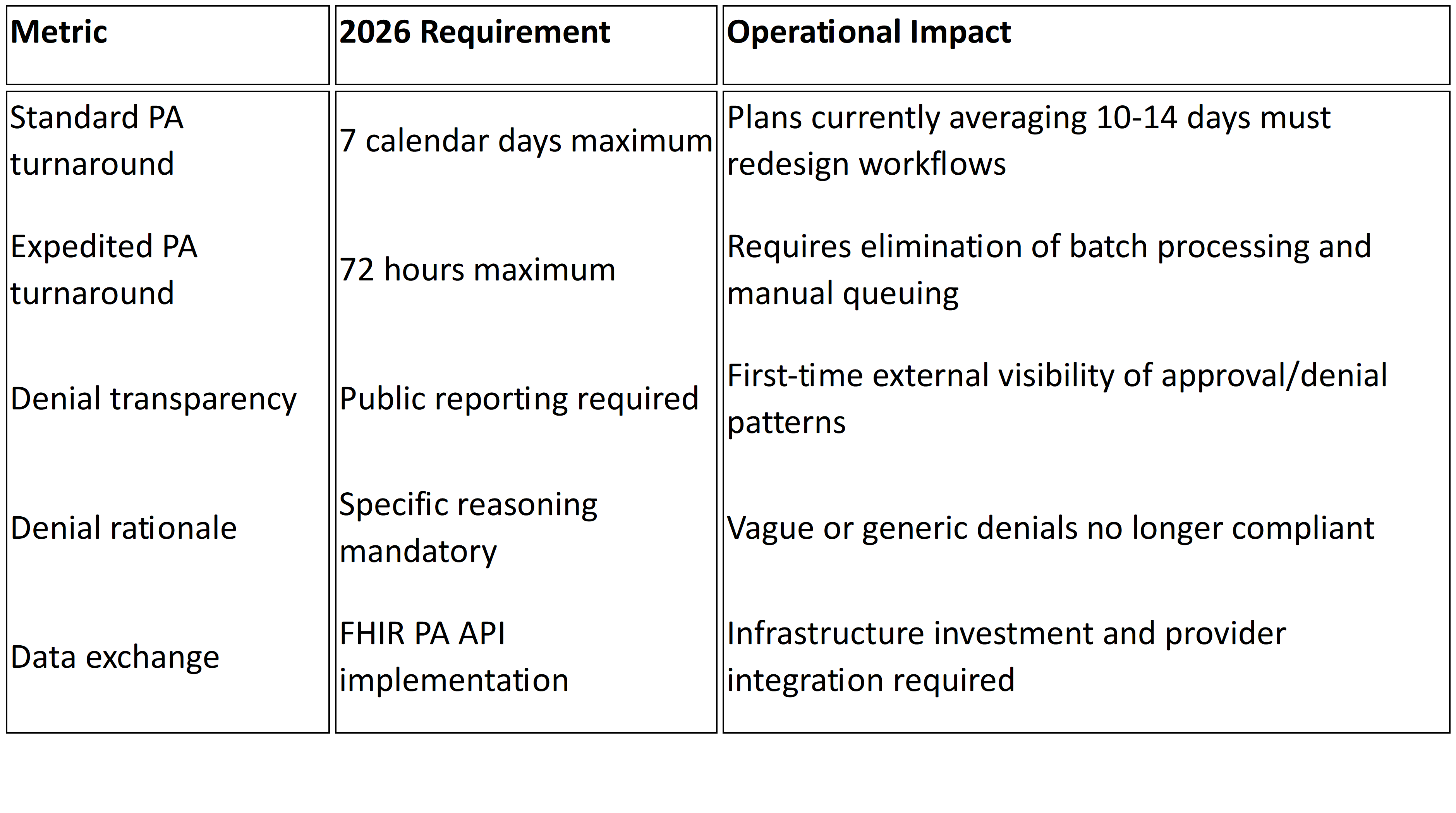
- Automated Triage and Rule Engines: Integrated workflows allow for low-complexity cases (e.g., recurring DME, imaging) to be auto-approved based on clinical criteria, reducing manual review volume. These rule engines must be dynamic and updated with CMS or plan-specific guidelines.
- Closed-Loop Communication with Providers: Integrated platforms should allow providers to receive immediate feedback on missing information and upload documents within the same system. This reduces rework and eliminates the “black box” effect of UM decisions.
- Post-Decision Data Sync: Authorization decisions must sync with claims systems in real-time, ensuring downstream claims are processed accurately against UM determinations—reducing post-payment denials and provider abrasion.
The Payoff: Efficiency, Experience, and Compliance
Plans that invest in integrated UM workflows aren’t just modernizing—they’re reaping returns.
- Reduced Denial Rates: Integrated eligibility and clinical data reduces avoidable denials by 15–30%.
- Shorter Turnaround Times: Real-time data eliminates delays from manual validation, cutting review times from days to hours.
- Lower Appeals Volume: Fewer preventable denials reduce administrative strain and provider frustration.
- Improved Audit Readiness: A single source of truth for decision rationale and documentation simplifies CMS compliance.
- Better Member Outcomes: Timely decisions enable timely care—reducing preventable ER visits, hospitalizations, and member grievances.
The global utilization management software market was valued at $15.21 billion in 2023 and is projected to reach $44.25 billion by 2031, growing at a compound annual growth rate (CAGR) of 18.25% from 2024 to 2031 2. This rapid growth underscores the increasing reliance on technology to address UM inefficiencies.
Additionally, in the U.S., the drug utilization management market is expected to reach $60.68 billion by 2030, with a CAGR of 7.3% from 2024 to 2030. Physicians handle an average of 19.7 prior authorizations per week, highlighting the significant administrative burden these tools create in clinical practice3.
The Road Ahead: Don’t Wait for the Perfect Platform
Some payers hesitate to overhaul their UM systems, fearing the cost or disruption of a full platform migration. But full transformation isn't required to make progress. Many integrations—especially eligibility, clinical document parsing, and provider feedback loops—can be layered onto existing systems through middleware, APIs, and smart automation tools.
The key is to stop treating UM as a static function and start treating it as a dynamic, data-enabled workflow. Because at its core, utilization management is not about saying "no." It's about saying "yes"—to the right care, at the right time, backed by the right data.
1 Exhausted by prior auth, many patients abandon care: AMA survey